Hormone Blockers are Very Dangerous Drugs
Exposing the dark history behind puberty blockers like Lupron.
Story at a Glance:
•Irreversible hormone blockers have dozens of severe side effects which affect between 5-50% of users. Millions have been injured by these drugs, and dozens of lawsuits have been filed by those they permanently disabled.
•Originally approved as an end of the line option for advanced prostate cancer, their use skyrocketed once they were priced so thousands of dollars could be made each time they were administered.
•A wide range of dubious uses were then concocted for these drugs such as treating a wide range of gynecologic conditions and blocking puberty.
•WPATH writes the guidelines for transgender medicine and exuberantly endorses giving hormone blockers to children while simultaneously denying and downplaying the dangers of this practice. Recent leaks revealed WPATH knows how dangerous this is and that they are in fact conducting a giant experiment.
Providing transgendered children “puberty blockers” is currently one of the most controversial areas in medicine. Remarkably, little knowledge exists about the safety of these drugs (e.g., when I’ve asked liberal colleagues who support these drugs if they were aware of their dangers, they genuinely shared that they were not aware the drugs had any clinically significant side effects).
Given that hormonal blockers are amongst the most dangerous drugs on the market, I feel it is essential to bring light to the people who they have harmed, and the scandalous 40-year saga that has allowed them to be unjustifiably used for a wide range of medical conditions.
How Hormonal Blockers Work
There are various ways you can block the production of hormones in the body. Since the signal to produce sex hormones (e.g., estrogen and testosterone) begins in the brain, cutting that signal off mainly eliminates the body’s production of hormones. The most potent hormonal blockers, the GnRH agonists, work by overstimulating the brain’s GnRH receptors so that they become “burned out” and no longer respond to the natural release of GnRH in the body, thereby short-circuiting the body’s production of sex hormones (which in many cases is a permanent deactivation).
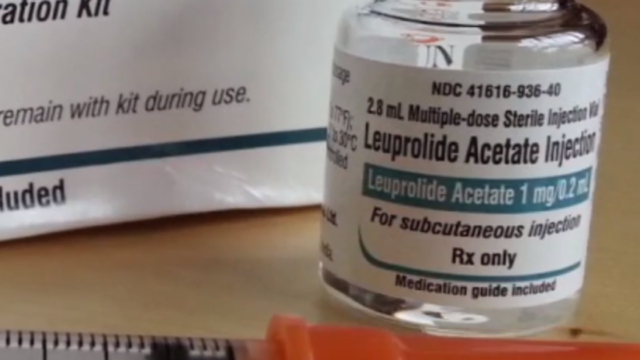
Note: A variety of different GnRH over-activators are sold, with Lupron, Vantas and Supprelin being the most widely used. Additionally, various drugs, such as Orilissa, instead function by directly blocking the GnRH receptor. Henceforth, I will focus on Lupron.
Testosterone, known to fuel prostate cancer growth, prompted extensive research into reducing its levels. Initially, countering testosterone with an estrogen analog called DES was promising. However, DES was withdrawn due to its severe adverse effects, which included harms to both the children and grandchildren of mothers who took it.
In 1984, a study compared Lupron (which chemically castrates males) to DES for advanced (likely fatal) prostate cancer, finding similar side effects and a slight increase in survival rates. This led to Lupron being approved as an alternative treatment for advanced prostate cancer despite FDA concerns about the study’s flaws and an incomplete understanding of Lupron’s metabolism.
Since that time, a myriad of additional dangers from the drug (e.g., an increase in fatal heart attacks or diabetes) have been uncovered, some of which suggest its reduction in prostate cancer deaths were due to it killing them from something else first.
Over time, Lupron’s usage has broadened beyond advanced prostate cancer to encompass various conditions, including advanced breast cancer, endometriosis, and fibroid pretreatment before surgery. Moreover, its off-label applications have proliferated, ranging from managing gynecological issues to assisting in in-vitro fertilization (IVF) protocols and chemical castration for sex offenders.
Hence, while these drugs were initially developed for men (i.e., prostate cancer), they are frequently given off-label to women. This, for example is why Lupron’s FDA insert states its only indication is for the palliative treatment of advanced prostate cancer, but it simultaneously warns against pregnant women taking it (even though it’s also used for egg harvesting)
In turn, despite having been on the market for decades, there is very little evidence to show these drugs actually benefit those who take them.
This hence raises the question—why on earth are these drugs so popular?
Selling Lupron
Lupron’s manufacturer faced a rather significant challenge—how could they get doctors to begin prescribing a hazardous and ineffective drug? They accomplished this through one of the most overt acts of physician bribery I’ve seen in American medicine.
Initially facing sluggish sales, Lupron’s manufacturer found a loophole in chemotherapy drug pricing, reformulating Lupron into a long-acting monthly shot for direct administration by urologists. This move allowed them to profit from marked-up prices, exploiting Medicare payments that soared to $1,200 per shot. Bribes and free samples were handed out to urologists to sweeten the deal, though this illegal practice eventually led to an $875 million fine.
The drug’s profitability enticed American urologists to adopt Lupron for increasingly benign prostate cancers, resulting in treatments costing nearly a billion dollars annually by the late 1990s. Medicare payments accounted for 40% of urology practices’ income. Medicare’s intervention in 2001 and 2003 led to reimbursement cuts, curbing Lupron’s excessive use and prompting a drop in inappropriate hormonal treatment rates for prostate cancer (leading to many urologists reporting their income had been halved).
Note: one survey found 53% of the urologists who did not believe prescribing Lupron benefitted certain prostate cancer patients still prescribed the drug to them.
Despite concerns about efficacy, Lupron’s profitability captured other medical specialties, leading to a surge in off-label uses, notably among obstetricians and gynecologists. This proliferation persisted despite poor data on Lupron’s efficacy for gynecological conditions and its exorbitant pricing, with patients often facing bills exceeding $10,000 for a single injection.
The significant markup on Lupron underscores questionable prescribing practices and raises doubts about the drug’s actual value. Patients experiencing adverse effects often encounter disbelief from negatively incentivized doctors, highlighting challenges in obtaining proper treatment and support. These issues underscore the need for greater transparency and ethical standards in pharmaceutical practices to safeguard patient welfare.
Lupron Lawsuits
Due to Lupron’s toxicity, many users have experienced severe and lasting incapacitation, leading to numerous lawsuits. This, in turn, may have deterred competitors from entering the market due to the substantial financial risk associated with potential lawsuits.
Despite numerous lawsuits against Lupron’s manufacturer and prescribing doctors, few have succeeded, even when cases involved clear harm caused by the drug being used for experimental or unapproved purposes. Many individuals injured by Lupron believe that the manufacturer’s extensive legal defenses (funded by the immense profitability of the drug), including alleged actions such as paying off judges or securing gag orders in settlements, make it nearly impossible to win a case. Consequently, many have struggled to find attorneys willing to take on their cases.
Lupron Toxicity
My longstanding interest in understanding pharmaceutical injuries has led me to conclude that Lupron is one of the most dangerous drugs on the market, based on the multitude and severity of reported injuries. Despite growing public pressure against Lupron in the late 1990s, efforts to collect evidence of its harm, such as the National Lupron Victims Network, faced obstacles and even disappeared mysteriously before publishing collected data.
In my research within Lupron support groups, I’ve found that women comprise the largest group of injured individuals, followed by those who took the drug to halt premature puberty, then men, and finally, transgender individuals. Many who took Lupron during puberty are experiencing adverse effects decades later, leading to concerns about similar long-term effects in transgender youth receiving puberty blockers. Notably, specialist reviews have highlighted the lack of controlled studies on Lupron’s use for early puberty or height enhancement, relying instead on expert opinion.
Some of the most commonly reported side effects of Lupron include:
- Significant decrease in bone density, leading to fractures and chronic dental issues such as teeth cracking and unexpected fractures even from minor stressors. This bone loss can occur rapidly and may emerge years after taking Lupron.
- Long-term or permanent damage to female menstrual cycles, with many experiencing failure to return to baseline ovarian function even one year after stopping Lupron. Other hormonal issues like permanent weight gain, abnormal menses, hot flashes, and vaginal atrophy are also frequent.
- Sexual dysfunction, with high rates of impotence reported in males and significant decreases in sexual desire, interest, and intercourse observed in some studies.
- Psychiatric conditions like depression, anxiety, severe mood fluctuations, dysphoria, rage, and suicidality are common after Lupron usage.
- Cognitive dysfunction, including memory loss and brain fog, is frequently reported, particularly among women receiving IVF treatments.
- Heart conditions like coronary heart disease, myocardial infarction, strokes, and sudden cardiac death have been associated with Lupron usage, especially in men.
- A study of more than 3000 women found that 76.7% reported joint pain and severe pain throughout the body is commonly reported in support forums.
Because of Lupron’s toxicity, condensing the thousands of heartbreaking injury reports I’ve encountered into this article was incredibly challenging.
Note: the FDA inserts for Lupron (summarized here) reported recipients experienced dozens of severe side effects at rates ranging from 5% to 50% depending on the symptom.
WPATH
Evidence-based medicine was created so that harmful and irrational dogmas within the medical field could be overturned by scientific evidence. While this was initially helpful, the process gradually became corrupted as the pharmaceutical industry realized doctors could be made to believe only the “best” evidence should be trusted and the groups purveying the “best” available evidence (e.g., the premier medical journals) could be easily bought out.
A key part of the push to buy out the “best” evidence has been to create authoritative guideline committees that are tasked with evaluating the existing scientific evidence and coming to a consensus over what constitutes the best practice of medicine. This process is fairly easy to corrupt since the industry can simply pay off the committee.
Take, for example, the handling of COVID-19 treatments. Despite ample evidence supporting the efficacy of affordable options like ivermectin, America’s corrupt (Fauci-appointed) committee chose to only recommend ineffective but expensive treatments like Remdesivir. This pattern repeats in other areas, such as statin usage guidelines, where industry influence skews recommendations to benefit pharmaceutical companies rather than patients.
In the realm of transgender medicine, guidelines set by organizations like the World Professional Association for Transgender Health (WPATH) heavily influence medical practice. Their guidelines advocate for the use of puberty blockers, such as GnRH analogs like Lupron, in various scenarios:
- They recommend administering these drugs at the earliest signs of puberty in transgender children, arguing that early intervention provides greater benefits.
- Puberty blockers are suggested as a temporary measure for adolescents who have undergone some puberty changes but are hesitant about starting hormone therapy.
- They are endorsed for individuals distressed by their body’s menstrual cycles or penile erections, as these drugs alleviate such discomfort by halting menstruation and suppressing testosterone.
- In cases where males seek to achieve female hormone levels, puberty blockers are presented as a solution.
- While they acknowledge the dangers of the cheaper hormonal therapies, they consistently downplay and dismiss the dangers of the more lucrative GnRH analogs.
Those guidelines are troubling for multiple reasons. Due to recent public scrutiny, even more ominous information has come to light in the form of leaked internal documents and correspondence from WPATH.
These leaked documents from WPATH reveal concerning insights into their advocacy for puberty blockers in transgender care:
- They admitted uncertainty about the long-term consequences, essentially treating the use of blockers as a giant experiment.
- Acknowledged significant side effects in children, including permanent loss of libido or orgasm ability, and emotional developmental hindrances.
- Despite claiming reversibility, they knew Lupron’s effects were often irreversible.
- Children receiving blockers were deemed too young to grasp the risks, yet WPATH sought to start treatment as early as possible.
Given all the things I’ve seen the pharmaceutical industry repeatedly do to make money during my lifetime, very few things surprise me these days. Nonetheless, even I was a bit taken aback when I discovered through these documents that there has been a push to affirm “plural identities” (multiple personalities) within WPATH. In turn, there are numerous cases which have been presented at WPATH conferences (e.g., under the umbrella of UCSF—one of America’s premier medical institutions) where each personality of an individual with split personalities was assessed for its sentiments on beginning a gender transition and at least one instance where some of the personalities did not consent but the transition was nonetheless deemed “ethical” and proceeded.
Note: the origins of the puberty suppression experiment stemmed from transgender adults’ dissatisfaction with their transition outcomes and a theory that preventing puberty could improve their final appearance. While it was acknowledged this would lead to inappropriate interventions (e.g., for someone who later realized they didn’t want to transition), they deemed the potential benefit (e.g., a more feminine appearance later in life) outweighed that risk.
Conclusion
The persistence of Lupron on the market despite its well-documented dangers and questionable efficacy is not just perplexing; it’s a testament to the flaws deeply entrenched in our healthcare system. It’s reminiscent of the ongoing battle with COVID-19 vaccines, where concerns over safety and efficacy clash with steadfast defense from regulatory bodies.
But amidst this turmoil, a silver lining emerges. The COVID-19 crisis has served as a wake-up call, exposing the cracks in our medical infrastructure and prompting a reevaluation of longstanding beliefs. Now, discussions once relegated to the fringes—like the potential risks of vaccines such as Gardasil or the historical ties between childhood vaccines and infant deaths—are being thrust into the spotlight.
As scrutiny intensifies, so too does the pressure on institutions like WPATH, whose leaked documents have peeled back the curtain on the reckless administration of puberty blockers.
More importantly, since the issue has been politicized, a lot of people are willing to listen, and major groups (e.g., numerous Republican states and England’s National Health Service) are now responding to public pressure and prohibiting the use of these drugs. Similarly, certain states are making it easier to sue doctors who give puberty blockers to children. As lawsuits against doctors prescribing puberty blockers to children increase, their medical malpractice insurance costs are soaring, making it financially unsustainable to continue administering these drugs. This shift underscores a growing acknowledgment of the risks associated with puberty blockers and signals a turning point in medical practice.
Yet, the battle is far from over. As our awareness grows, so does the urgency to address the broader implications of pharmaceutical overreach. With each person’s contribution to the cause, we edge closer to a future where patient safety takes precedence over profit margins—a future where no one suffers at the hands of a healthcare system meant to heal, not harm.
https://www.midwesterndoctor.com/p/hormone-blockers-are-very-dangerous
